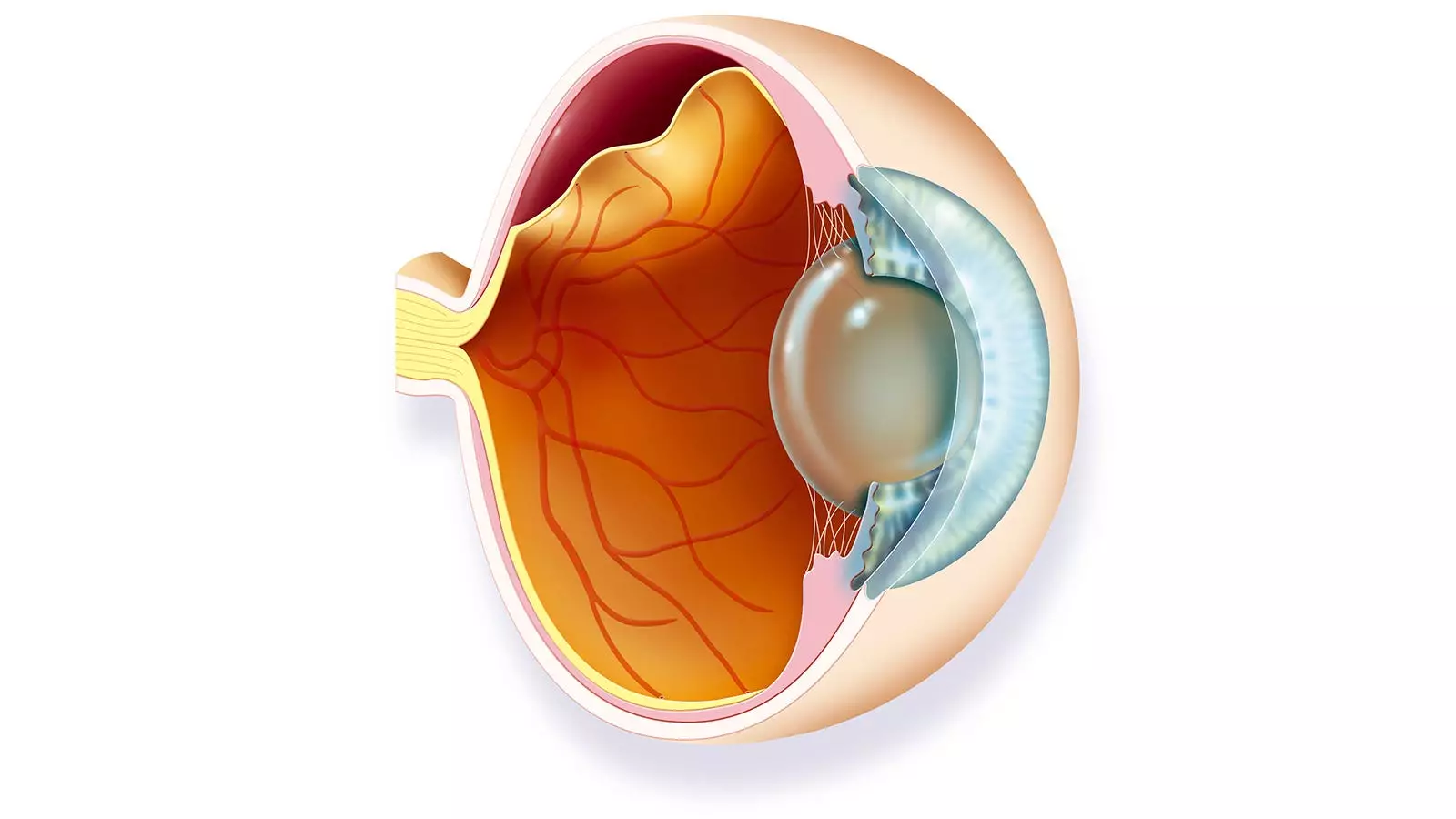
Rhegmatogenous retinal detachment (RRD) is a condition noted for its potential to cause significant vision loss, and it primarily affects older adults and individuals with specific risk factors such as extreme nearsightedness or prior ocular trauma. As the most prevalent type of retinal detachment, RRD occurs when a tear or hole develops in the retina, allowing fluid to accumulate beneath it, consequently separating the retina from the underlying layers. The urgency of treatment cannot be overstated, as early intervention is critical to restoring vision and preventing long-term damage. One recent retrospective cohort study has brought to light critical insights regarding the correlation between socioeconomic determinants and the severity of RRD at the time of clinical presentation.
According to findings from a study conducted with 700 patients undergoing primary repair for uncomplicated RRD at the Wilmer Eye Institute, socioeconomic factors significantly impact the presentation of RRD. The Area Deprivation Index (ADI) was utilized as a measure of socioeconomic disadvantage, revealing that a higher ADI correlated with worse visual acuity and greater likelihood of fovea-involvement during diagnosis. Specifically, each decile increase in the ADI resulted in a 14% increase in the odds of presenting with impaired vision. Such statistics emphasize how patients living in more disadvantaged neighborhoods face compounded barriers, effectively delaying access to timely and necessary care.
Moreover, fluctuations in per capita income also carried notable implications for treatment outcomes. A $1,000 increase in income per capita was associated with lower odds of presenting with poor vision. This connection underscores how income disparity can hinder access to healthcare resources, compelling individuals from lower socioeconomic backgrounds to postpone seeking help until their conditions become critical.
The interplay between neighborhood characteristics and health outcomes further complicates the discussion. The study highlighted a perplexing correlation between the percentage of workers who commuted by car and the odds of presenting with serious vision problems. As the ratio of car-dependent commuters grew, so too did the likelihood of patients arriving with advanced RRD at a later stage. This could suggest that areas with limited public transportation options may inadvertently restrict access to healthcare for individuals reliant on alternative means of commute.
The research team posited that neighborhoods with a high proportion of driving commuters often lack adequate public transit facilities, making it challenging for those without personal vehicles to reach medical care. This dynamic forms a critical component of understanding health disparities, particularly among marginalized groups who may not have the privilege to navigate transportation obstacles effectively.
Dr. Sally S. Ong, one of the study’s co-authors, pointed out that the ramifications of delayed care among disadvantaged populations could be severe. Patients might defer seeking medical attention for extensive periods—days, weeks, or even months—due to financial or logistical barriers. Such delays can not only exacerbate the condition at hand but also complicate future treatments, raising the risk for additional retinal detachments.
Moreover, the symptoms of RRD, such as peripheral dark shadows in vision, may not prompt immediate action from patients who are unaware of the severity of their condition. The lack of awareness among at-risk populations, coupled with socioeconomic barriers, necessitates urgent action from clinicians. Enhanced efforts to educate patients about the importance of early intervention could significantly alleviate treatment delays and resultant health complications.
Addressing these disparities in access to treatment is of paramount importance. Clinicians should be proactive in fostering understanding among disadvantaged communities regarding the importance of promptly addressing vision problems. Collaborating with social workers and community health organizations to assist patients with transportation and work-related obstacles can pave the way for equitable healthcare access. Furthermore, public health campaigns promoting awareness about the signs of retinal detachment may empower individuals to seek help earlier.
Alongside enhancing patient education, further research into the neighborhood dynamics affecting healthcare access is critical for formulating targeted interventions. By understanding the specific barriers faced by various populations, healthcare providers can develop strategies tailored to those needs. As health equity continues to be a pressing issue in healthcare, tackling the socioeconomic determinants influencing conditions like RRD could lead to better outcomes for all patients.
The relationship between social determinants and the severity of RRD reinforces the urgent need for systemic change in how healthcare is accessed across different demographics. Effective strategies are essential to reduce treatment delays and improve visual health outcomes. By recognizing and addressing the multifaceted barriers that contribute to delayed care, we can move towards a more equitable healthcare system that prioritizes the well-being of all individuals, irrespective of their socioeconomic status.

Leave a Reply