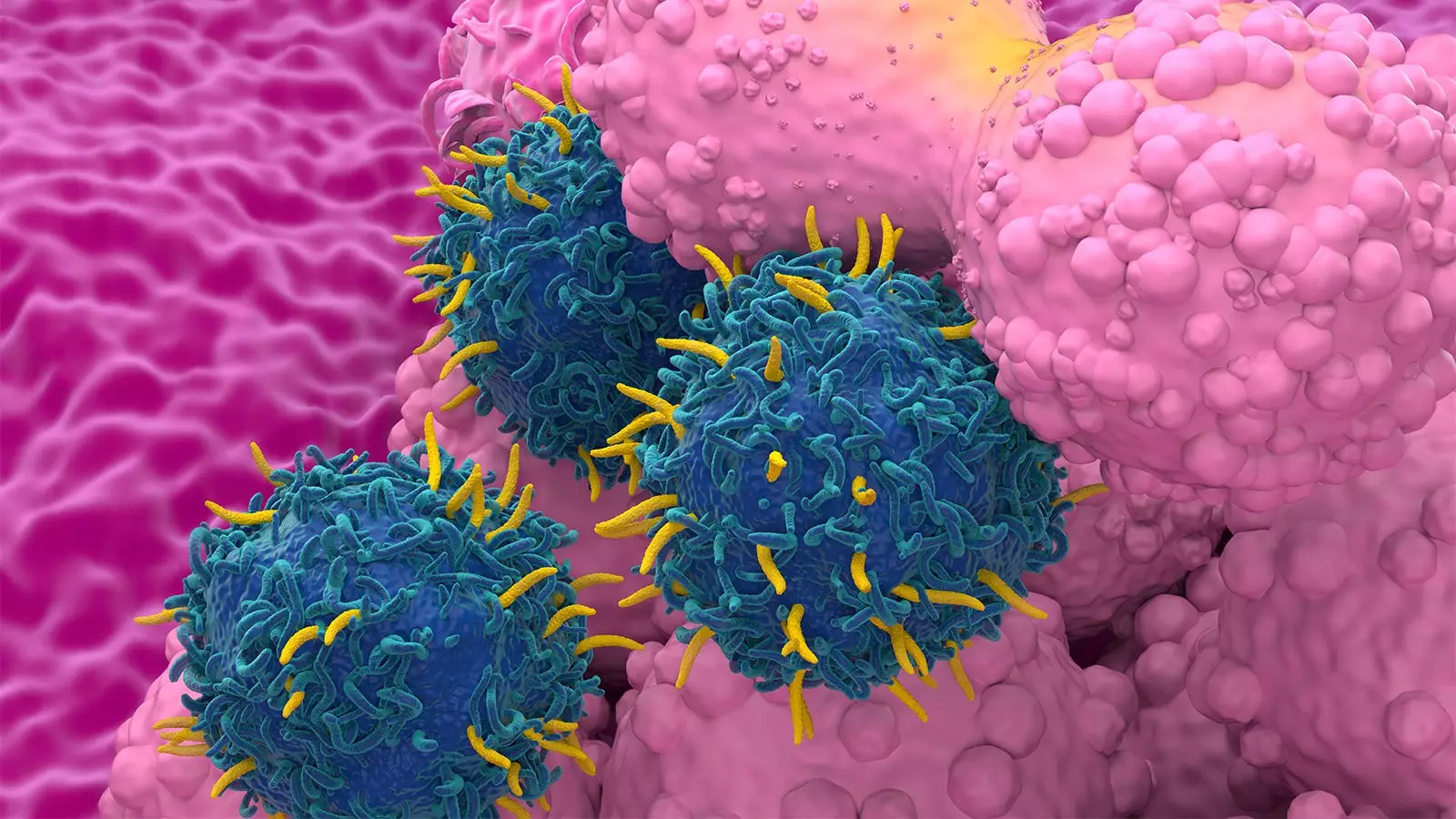
Chimeric Antigen Receptor (CAR) T-cell therapy has emerged as a groundbreaking treatment for certain types of blood cancers, specifically lymphoma and multiple myeloma. The ingenuity of this treatment lies in its ability to harness the patient’s own immune system by genetically modifying T-cells to target cancer cells more effectively. Though the therapy has garnered considerable attention for its potential benefits, concerns have surfaced regarding the risk of developing second primary malignancies (SPMs) in patients undergoing this treatment. A recent systematic review and meta-analysis seek to assess this risk and offer a comparative analysis with traditional treatment modalities.
The analysis examined data from over 5,500 patients with a median follow-up duration of approximately 22 months, revealing an overall SPM rate of 5.8%. Notably, this figure aligns closely with SPM rates reported for conventional standard-of-care (SOC) cancer therapies. Delving deeper into the data, researchers found that the SPM incidence did not fluctuate based on the specific type of cancer being treated or the CAR T-cell products utilized. This stability across diverse contexts raises intriguing questions about the relative risks associated with CAR T-cell therapy compared to traditional approaches.
A significant observation from the analysis was the impact of study setting on the SPM rate. Patients participating in clinical trials were found to have a higher SPM risk compared to those undergoing therapy in real-world settings. Notably, longer follow-up periods also correlated with elevated SPM rates, suggesting that the duration of patient monitoring plays a critical role in SPM detection. Furthermore, it was noted that those who had undergone multiple treatment lines before receiving CAR T-cell therapy were more likely to develop SPMs.
The methodological rigor of the meta-analysis offers a solid foundation for understanding SPM risks, yet it also highlights the necessity for careful interpretation of the data. Dr. Kai Rejeski, a prominent figure in this research, emphasized that the findings challenge the notion that CAR T-cell therapy inherently increases the risk of SPMs when compared to standard oncological treatments. Instead, the evidence suggests that pre-existing factors beyond the CAR T-cell intervention itself may largely dictate the likelihood of secondary malignancies.
This nuanced understanding brings attention to the black-box warning placed by the FDA on CAR T-cell therapies, which arose following reports of secondary malignancies. While such regulatory caution is prudent, it also underscores a critical need for patient education on the complexities involved in interpreting risk data associated with novel therapies. As healthcare providers navigate these discussions, a careful contextualization of the evidence will be crucial for patient reassurance and understanding.
Among the various factors investigated, previous treatment history emerged as a significant contributor to SPM development. Patients with a history of extensive therapy before CAR T administration had a numerically higher rate of SPMs. This observation raises the possibility that cumulative effects from prior cancer treatments could augment the susceptibility to secondary cancers.
Additionally, the research suggests that the health status of patients and their overall disease burden can significantly affect outcomes. It remains crucial for researchers and clinicians to delineate these variables in an effort to provide a comprehensive picture of SPM risks associated with CAR T therapy.
The authors of the meta-analysis rightly call for extensive long-term studies to provide a clearer understanding of the long-lasting effects of CAR T-cell therapy. While the current findings indicate that the SPM risk may be comparable to that of traditional therapy, it is essential to gather more data as patients move further into survivorship. Increased lifespans resulting from successful CAR T treatments could lead to a higher cumulative risk of secondary malignancies, necessitating ongoing monitoring and research.
As patients increasingly seek information regarding potential treatment risks, it is imperative that healthcare providers address these concerns with accurate, evidence-based communication. Rejeski aptly noted that while understanding potential risks is vital, it is equally important to weigh the possibilities that CAR T-cell therapy offers in terms of extending life and improving quality of life.
In summarizing the findings from the recent meta-analysis, it becomes apparent that the risk of second primary malignancies associated with CAR T-cell therapy does not significantly exceed that of standard cancer treatments. However, this should not diminish the importance of vigilance and comprehensive follow-up. As the field progresses, a balanced approach that weighs benefits against risks, informed by robust clinical data, will be key in optimizing treatment protocols for patients battling cancer. The evolving landscape of CAR T-cell therapy is not merely about survival, but also about ensuring long-term health and well-being for patients who choose this innovative treatment avenue.

Leave a Reply