The safety and side effects of contraceptive methods are critically important topics in women’s health. Recent findings from a Danish registry study have drawn attention to a concerning potential link between the use of levonorgestrel-releasing intrauterine devices (IUDs) and an increased risk of breast cancer among premenopausal women. With a follow-up period approaching seven years, the study offers insights that merit further discussion concerning hormonal contraceptives and women’s health.
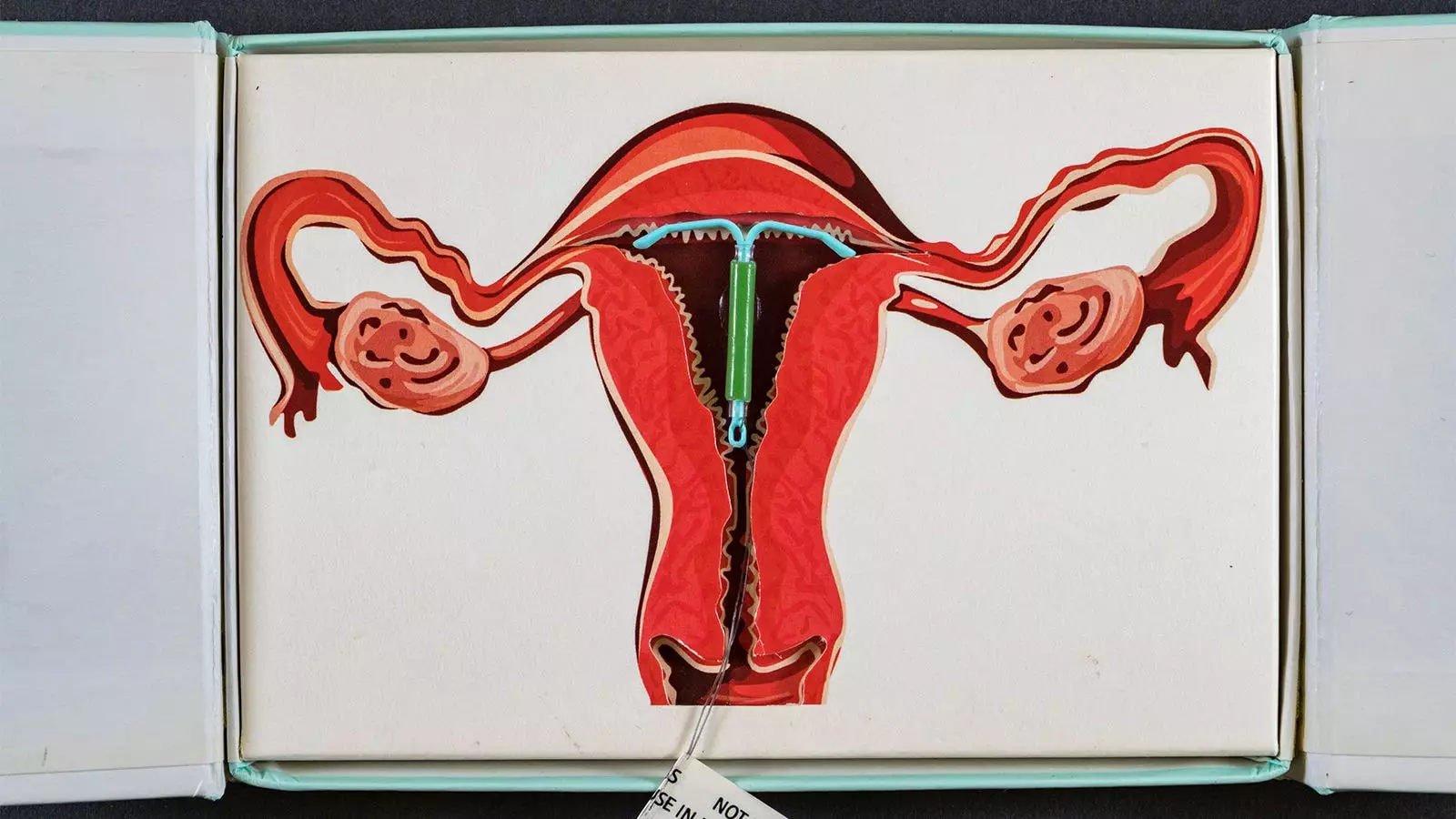
The research, led by Lina Steinrud Mørch, PhD, from the Danish Cancer Institute in Copenhagen, focused on women aged 15 to 49 who began using levonorgestrel-releasing IUDs for the first time between 2000 and 2019. A total of 78,595 users of these devices were compared to an equal number of non-users who had not used any hormonal contraceptives in the preceding five years. This careful matching aimed to ensure that the participants had similar baseline characteristics, such as age, reproductive history, and gynecological issues.
Throughout the study, researchers discovered that the long-term use of these hormone-releasing IUDs was linked with a 40% increased risk of developing breast cancer. Notably, this risk intensified with prolonged usage — surging to 80% among those using the device for 10 to 15 years. While these results present a worrisome finding, it’s crucial to note that the study’s trend analysis did not yield statistically significant results.
According to the data collected, there were 1,617 new breast cancer diagnoses in total, with 720 cases among IUD users and 897 among non-users. The hazard ratios, a statistical measure used to compare the risk of an event occurring between two groups, indicated that LNG-IUD users faced a higher risk compared to non-users. Specifically, hazard ratios showed a modest increase in breast cancer diagnoses with durations of IUD use: for 0-5 years, the ratio was 1.3; between 5-10 years, it reached 1.4, and for more than a decade of use, it increased further to 1.8.
This means that the excess number of breast cancer diagnoses ranged from 14 per 10,000 users for those using the device for a short duration to a staggering 71 excess cases for those using it for the longest duration. However, it is worth noting that the non-significant P-value of 0.15 in the trend analysis signals that while there may be a difference in breast cancer rates, the evidence is not definitive, raising questions about the causal mechanisms involved.
The increasing adoption of levonorgestrel-releasing IUDs, particularly among younger women, necessitates thorough discussions about the potential benefits and risks associated with their use. As such, the findings underscore the importance of informed consent when choosing contraceptive methods. Healthcare providers should actively engage in conversations about these risks, especially for women with pre-existing risk factors for breast cancer or family histories of the disease.
It is also essential to consider the broader context of hormonal birth control and its association with breast cancer. Prior studies have linked hormonal contraceptives with increased risks of breast cancer, indicating a possible trend across various types of hormonal birth control. More specifically, recent research indicated that BRCA1 carriers who used any hormonal contraceptive faced a 29% greater relative risk of developing breast cancer.
Despite the noteworthy findings, the study has its limitations. The researchers acknowledged that some participants may have prematurely removed their IUDs, potentially underestimating the associated risk. Additionally, the effects of unmeasured confounding factors could also play a role, indicating that causation cannot be conclusively established based on this study alone. Hence, as with all studies in this realm, caution is needed when interpreting the results and making healthcare decisions.
Moving forward, further research is necessary to clarify the mechanism behind this association, explore potential risk factors, and determine whether specific subpopulations may be at higher risk. Until more definitive evidence is available, patients and healthcare providers should maintain an ongoing dialogue about contraceptive choices and associated health risks.
The connection between levonorgestrel-releasing IUDs and breast cancer, highlighted in this Danish study, raises significant concerns that warrant attention within women’s healthcare. As the dialogue around contraceptive methods continues to evolve, a balanced perspective that emphasizes both the benefits and risks is crucial for informed decision-making. Healthcare providers must remain vigilant in offering personalized advice, guiding women to make choices that align with their health needs and values.

Leave a Reply