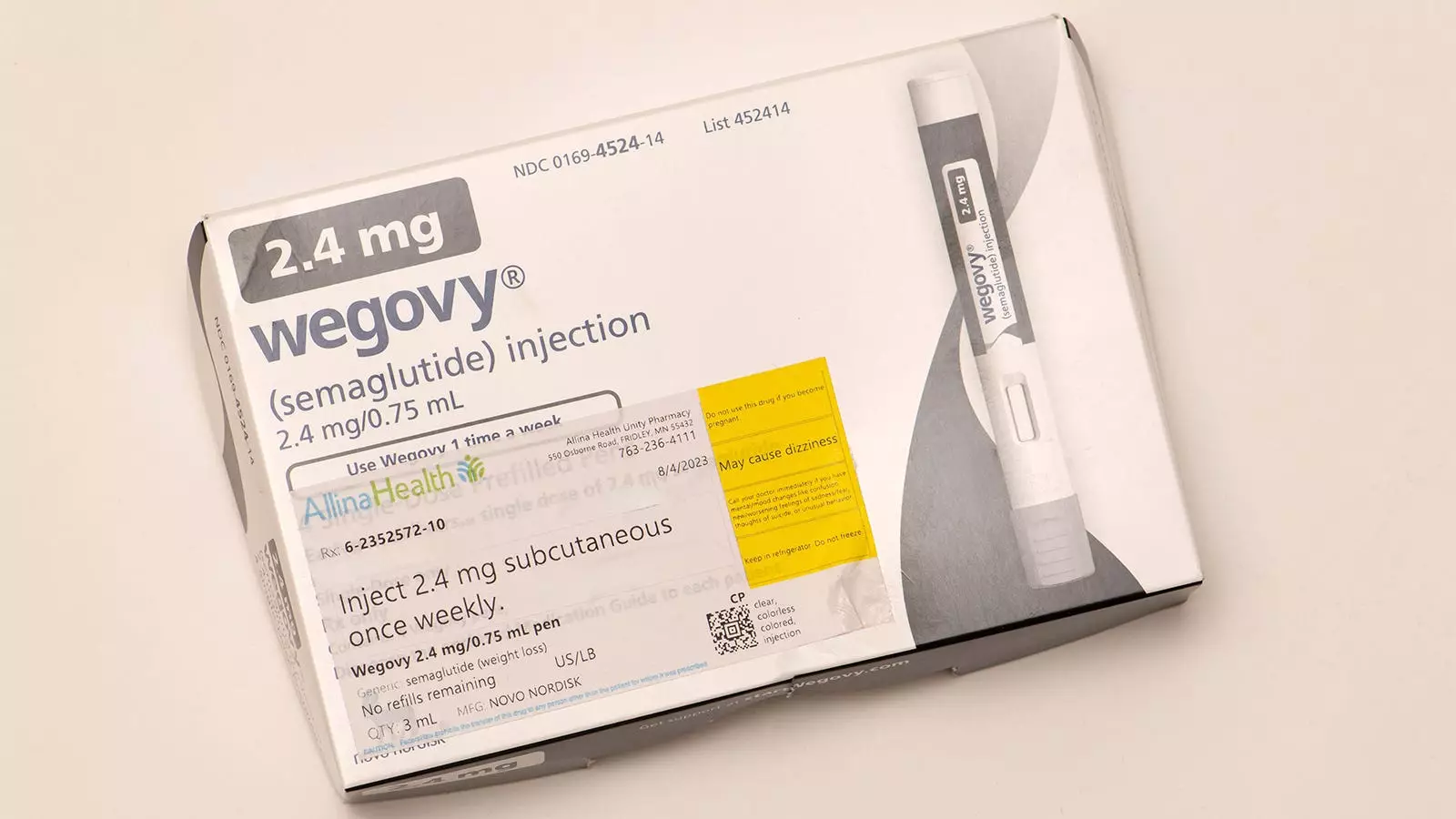
As childhood obesity rates rise dramatically, healthcare professionals are facing mounting pressure to address this pressing health issue effectively. Pediatric obesity is not merely a cosmetic concern; it is a disease with multifaceted complications that can lead to severe comorbidities such as diabetes, cardiovascular conditions, and psychological issues. Within this context, the introduction of GLP-1 receptor agonists, especially medications like semaglutide (brand name Wegovy), has sparked a wave of optimism. These medications have shown promising results in treating adolescent obesity when combined with intensive lifestyle interventions, improving not only physical health but also psychosocial aspects, such as self-esteem and emotional well-being.
Yet, while these developments are promising for adolescents, there remains a significant gap in treatment options for younger children, particularly those under 12 who are grappling with severe obesity. Despite the alarming prevalence of obesity-related risk factors in this age group, the lack of approved medications poses a considerable challenge, leaving health specialists with limited options to combat this epidemic.
The Potential Role of Liraglutide
Recent deliberations by the FDA regarding the possible approval of liraglutide for treating severe obesity in children aged 6-12 represent a pivotal moment in the fight against pediatric obesity. A recent trial published in the New England Journal of Medicine (NEJM) provides a glimmer of hope, demonstrating the drug’s efficacy and safety when paired with lifestyle intervention. The study followed 82 children over a 56-week period and identified an average 5.8% reduction in BMI among those on liraglutide compared to a 1.6% increase in the control group.
Despite the potential for liraglutide to change the treatment landscape for younger children, it is essential to approach its integration into clinical practice with caution. While the trial reported favorable outcomes, one must also consider that nearly 80% of participants experienced gastrointestinal side effects from the drug, although most were mild to moderate. Such findings underscore the necessity for further research to determine long-term safety and potential consequences of medication use on growth and development in pediatric patients.
In weighing the prospect of including liraglutide in treatment plans for young children, healthcare providers must engage in a detailed analysis of its risks and benefits. The potential advantages include significant reductions in BMI, possible enhancements in metabolic health, and theoretical psychosocial improvements derived from earlier studies in adolescents. However, these benefits must be contrasted with the potential risks. Unknown long-term effects, particularly concerning growth and height, raise red flags, as does the prospect of medication-induced weight regain post-treatment.
Interestingly, during the aforementioned study’s follow-up, children who had received liraglutide experienced a weight regain of nearly all lost pounds after stopping the medication, indicating a rebound effect that complicates long-term management strategies. The need for daily injections is another consideration that could impact adherence and, consequently, treatment efficacy.
Individualized Treatment Approach
Severe obesity in children is far from a one-size-fits-all condition. Effective treatment must be individualized, considering a variety of factors including age, present health conditions, and psychosocial aspects of the patient. Within this framework, introducing GLP-1 receptor agonists like liraglutide could serve as an adjunct therapy, provided that comprehensive lifestyle interventions are a cornerstone of the treatment plan.
However, due to the changing landscape of pediatric obesity research, there are valid concerns regarding the potential for pharmacological interventions to overshadow essential lifestyle changes. It is crucial that treatment protocols continue to prioritize behavioral health interventions, ensuring families are equipped with the strategies they need to foster lasting change.
The ongoing exploration into pharmacological options for treating pediatric obesity reflects a broader commitment to address this complex health crisis. With continued research and potential FDA approvals on the horizon, medical professionals are eager to find effective, safe solutions for their young patients. As we await further developments, there is a palpable sense of hope among those dedicated to improving the health of the next generation. It is essential we proceed cautiously, keeping the best interests of these vulnerable patients at the forefront of all decision-making processes. The road ahead may be challenging, but the medical community’s commitment to finding effective solutions remains unwavering.

Leave a Reply